One of the biggest problems in total hip replacement is the bone loss that occurs at the proximal part of the femur. This occurs because of a phenomenon called stress shielding, which eventually leads to loosening of the prosthesis. Therefore, the primary concern with the design of total hip replacement implants is to ensure load is transferred in such a way to minimize stress shielding and bone resorption. Despite the general success of this operation, aseptic loosening due stress shielding has led to an increase in the number of failed total hip replacements. It is therefore of great clinical significance to improve the design, materials, and survivorship of hip implants to reduce the rate of total hip failures and revision. We can do this by gaining insight as to how bone adapts itself in response to mechanical loading environment and developing implants that are responsive to bone’s remodeling needs.
Assuming the implant is properly press fit and bonded to bone (implant has achieved secondary stability through osteointegration), the material and design of an implant basically determine how load is transferred from the implant to bone. How load is transferred has nothing to do with surgeon technique, but everything to do with the mechanical properties and design of the implant. For long term success of any arthroplasty, load must be distributed just the right way for the bone not to resorb, or remodel negatively. Bone is a live structure and basically adapts and reinforces itself wherever it experiences lines of stress and conversely resorbs itself wherever lines of force are not present. This is called Wolfe’s law.
With respect to stress shielding and bone resorption, the stiffer portions of the implant bond well to bone with good bone ingrowth, however, portions of bone proximal to this area will not experience natural stresses and therefore resorb and disappear, eventually leading to aseptic loosening.
Conversely, if the implant is too flexible, there will be too much micro-motion at the implant-bone interface. This leads to fibrous ingrowth, which also leads to aseptic loosening. Therefore, creating a hip implant with proper material properties and design such that the implant allows proper load transfer between implants and bone is a Goldilocks problem. Too stiff is not good because it leads to stress shielding and bone resorption and thereafter loosening, yet too flexible directly leads to too much micro-motion and loosening. That is why we need implants that can be both stiff and flexible at the same time to solve the problem of loosening associated with load transfer.
Bone, a composite material, is strong and flexible. It has complex and elaborate designs on all scales, including at the nanometer scale where triple helices of collogen mix with calcium phosphate matrix and at the micrometer scale with lamellae of complex fibers around osteons. Wood has a similar anatomy with concentric rings and cross-grain patterns. These complex designs at the mesoscale level within the structure of bone and wood provide flexibility, strength, and toughness. Re-enforced concrete simulates a similar concept of introducing a framework of metal rebar within concrete to add tensile strength. These structures have one thing in common. They each have a complex framework of fibers, beams, struts, ribs, and planks, etc. that are embedded within the matrix to provide a tailored anisotropy. This may be the reason why bone and wood are not only anisotropic but also viscoelastic.
Current advanced technologies for femoral implants include functionally graded and porous metals, both of which create anisotropic properties. They accomplish this by manipulating the mechanical properties of the metal through alteration of the base metal’s cellular structure, at the microscopic level. This is done by changing geometry of the cell and increasing or decreasing porosity.
However, manipulation of cellular structure of metal creates vulnerabilities. Failure and cracks of cellular structures occur at the junction between the unit cell, which propagates throughout one or more structural elements to create a macroscopic fracture of the implant. The joints between the cells are the weakest link of cellular material as stress localizes in these regions to reduce the strength of the material. Additionally, with increased porosity, comes increased flexibility, which leads to increased micro-motion. Micromotion greater than 50 µm leads to fibrous union and aseptic loosening.
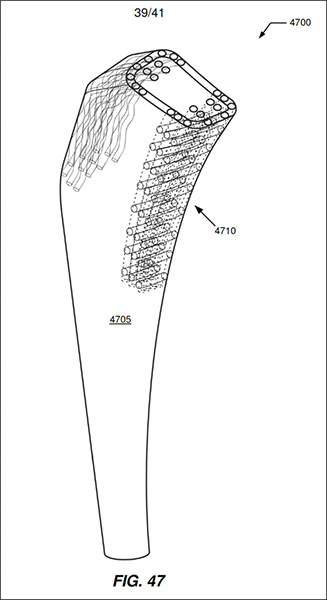
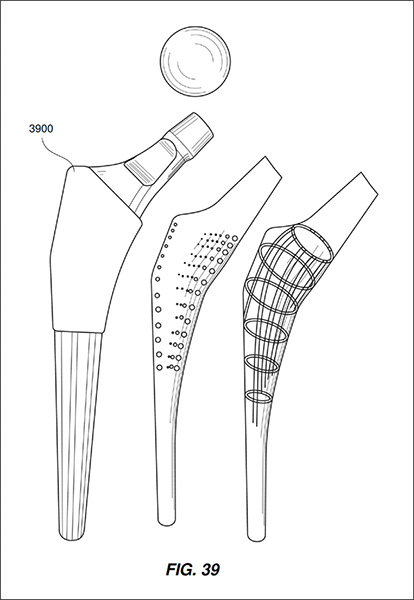
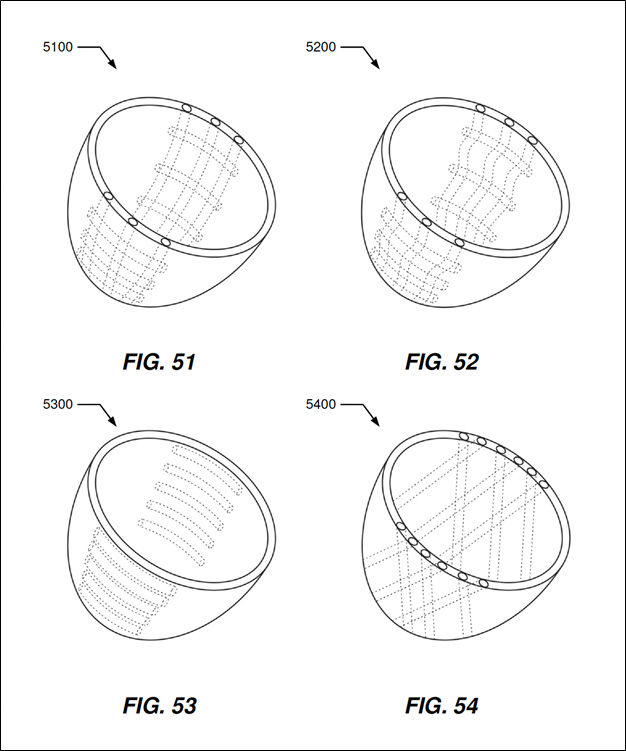
We suggest the idea of VARIABLE MATERIAL PROPERTIES PROSTHESIS through formation of a frameworks within the structure of the implant, similar in concept to what occurs in bone and wood and reinforced concrete. A framework, made of tubes, slabs, walls, columns, beams, struts, ribs, planks, and sheets can produce tailored anisotropic properties within the implant. Creation of a framework within an implant produces bulk anisotropic properties. This framework can be made of different material than the metal matrix in which it is embedded. The framework material may include such material as glass, carbon, high strength polymers, aramid- Kevlar, silicon carbide, fine fibers of pure carbon (graphite and carbon nanotubes), nanotubes of boron nitride. This framework may be embedded in a matrix made of Stainless steel, Titanium, Cobalt chrome and Polymer implants.
Current femoral implant designs are either diaphyseal loading, metaphyseal loading or neck loading via a collar. Each of these strategies produces a different set of problems with stress shielding and bone resorption. However, with current computational and additive manufacturing capacities, we can lay (print) the framework within the implant purposefully to counteract areas of bone that see different kinds of stress. In doing so, we can create the advantage tuned anisotropy within the implant.
With this concept of the custom framework, implants can be created with spatially varying bulk anisotropic properties. This allows an infinite variety of tailored flexibility, strength, and toughness to meet the needs of the patient. This concept allows implants to be global or custom loading, instead of neck, diaphyseal and metaphyseal loading.
A perfect example of this is the medial calcar of the human femoral neck. This portion of the femur is designed by nature to resist compressive forces. Conversely, due to the abductor muscles, the neighboring greater trochanter is exposed to tensile stresses. We can create an implant with internal framework to meet these demands.