Conversation 1.
In the recent 2023 ISTA (International Society for Technology in Arthroplasty) meeting in New York, during a Panel session with high level medical device executives, an attendee asked a question to the following effect. “The adoption of robotics in total knee replacement is 15%. This is despite the many years of promotion and marketing. What do you believe is the future of robotics in orthopedics?”
The response from one of the vice presidents of the medical device companies was sharp and condescending. Something to the following effect. “You have no idea what you are talking about. We believe adoption of robotics in the next four years will be around 50%.” This response is rather emblematic of the relationship of the majority of orthopedic surgeons with the medical device companies.
The positive interpretation is that the medical device companies believe orthopods are smart, but not smart enough to know what they need. The negative interpretation is something like this: “you better be quiet and use what we have created because we have already spent hundreds of millions of dollars on the project and we are not about to scrap it because you (majority of orthopedic surgeons) do not like it.”
Conversation 2.
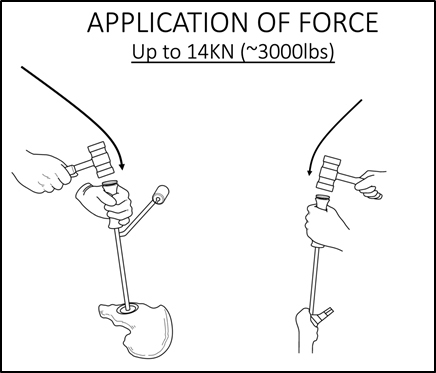
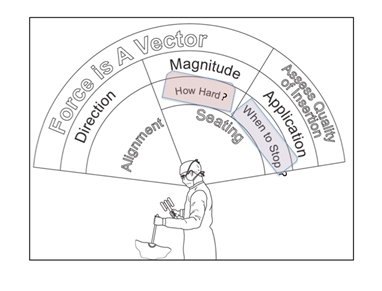
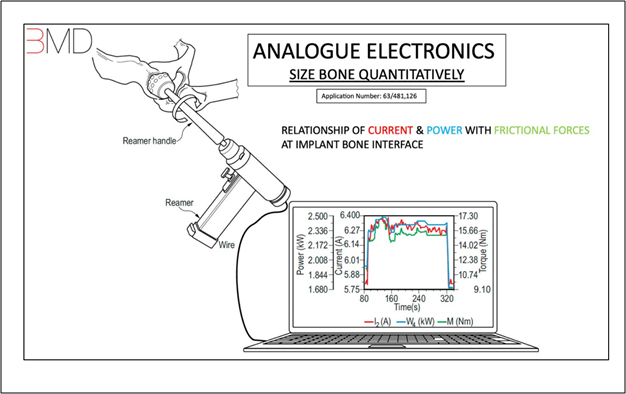
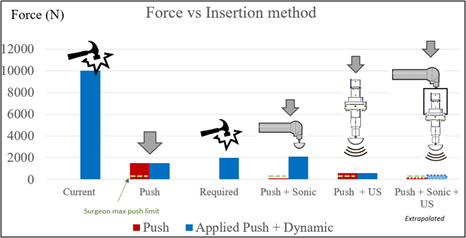
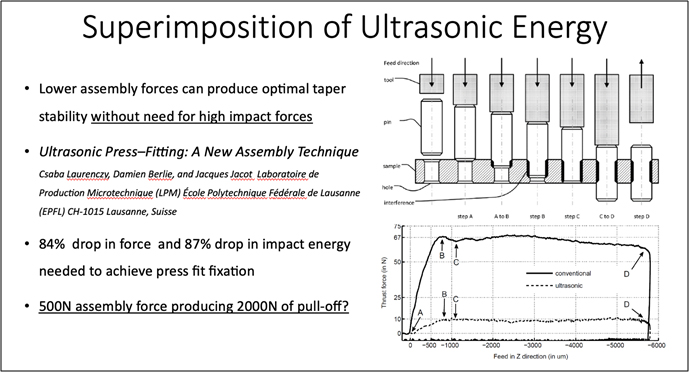
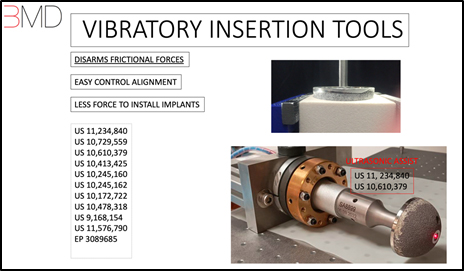
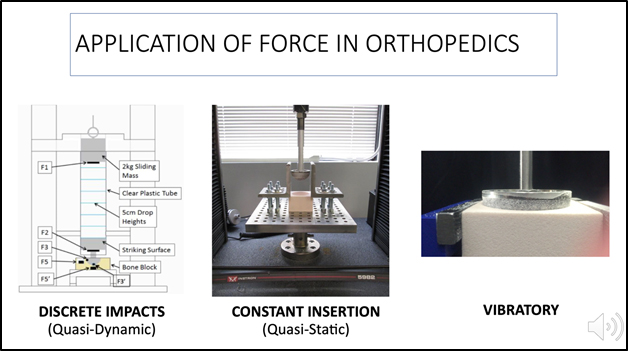
In the same panel meeting another attendee asked about the concept of digitization. The response from another executive was the following. “Digitization is the new GOLD. We are primarily interested in these projects”. This response is also emblematic of another problem in orthopedics. In this day and age of computers, data analysis and virtual reality the work of the orthopedic surgeon is still “Newtonian”- in that it involves application of force. In other words, we apply large amounts of force up to 10KN to 14KN to the patient’s body. This level of force typically shocks the uninitiated who come to the operating room to observe how a total hip replacement is done. Digitization and focus on the spatial relationships of implants will not help the primary problem that orthopedic surgeons have, which is the management and application of force. Here again there is a disconnect between the surgeon and the medical device executives.
These two conversations highlight a problem that has permeated our community. It has turned us, the orthopedic surgeons, into followers instead of leaders. This is not unusual as most of our inquisitiveness is beaten out of us during grueling residencies. And so, we put our heads down and do what we are told, even though deep down inside, we know we can do better.
This paper is about how we can (and should) do better for ourselves and our patients. It assumes a reality where we are raising our heads up and asking for the tools we need, to do a better job. Specifically, we will discuss the five major problems in total hip replacement, since this procedure is an aspect of orthopedics that has the largest infusion of technology, and yet major problems persist. We will touch on why these problems persist and how we can solve them.
PREAMBLE
Total hip replacement is one of the most successful operations dubbed the operation of the century. It is a $7 Billion industry with 1 million total hip replacements performed yearly around the globe, 500,000 in U.S alone. It has relieved pain for millions of people. However, it continues to have unsolved problems.
It is estimated that 13% of total hip replacements fail within ten years of index operation. Of these failures 50% occur due to aseptic loosening or periprosthetic fractures, which are the opposite sides of the same coin. These failures many times are catastrophic and cause pain, suffering and loss of functional mobility. When total hip replacements fail, a revision surgery is performed to correct the problem. Revision surgeries cost up to $2 Billion a year and the results are rarely as good as the primary procedure.
These problems persist despite major technological advances in robotics and navigation.
Adoption of Robotics in total hip replacement around the globe is even worse than adoption of robotic in total knee replacement and stands at 1%. Despite the vice presidents claims that in a few years 50% of arthroplasties will be done with robotics, orthopedic surgeons are clearly not convinced about the value of robotics, especially in total hip replacement.
In general, there are five major problems that plague total hip replacement surgery today.
These include:
1. Aseptic Loosening and Periprosthetic Fractures (two sides of the same coin)
2. Mal-positioning of implants
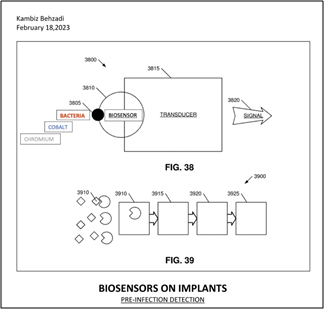
3. Infection
4. Leg length and Offset discrepancy.
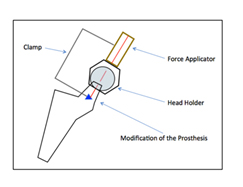
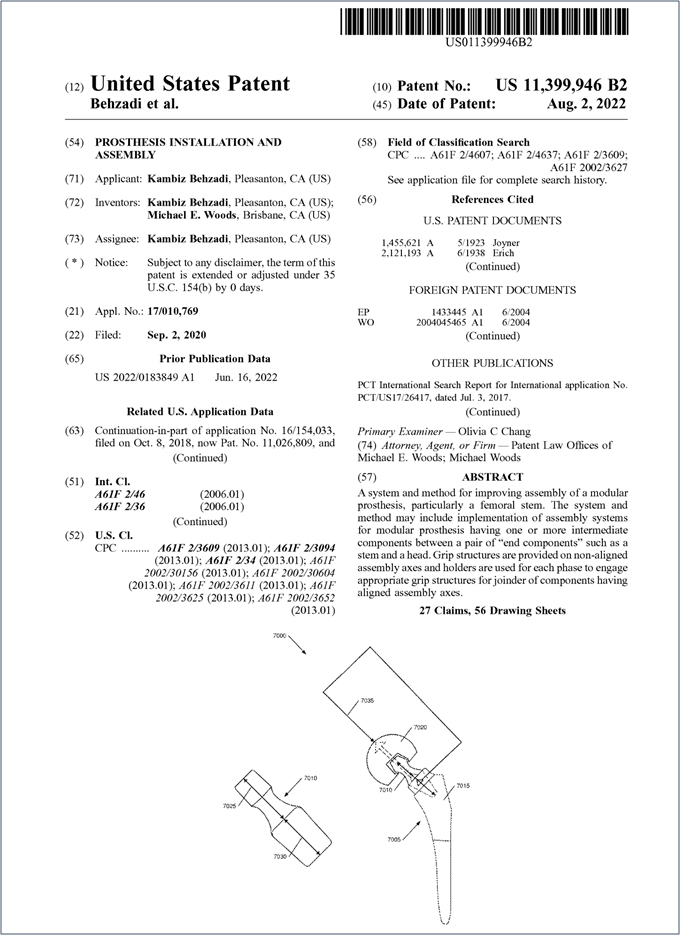
5. Metallosis and Trunnionosis (metal debris associated with modular implants).
In this paper we propose solutions to each.
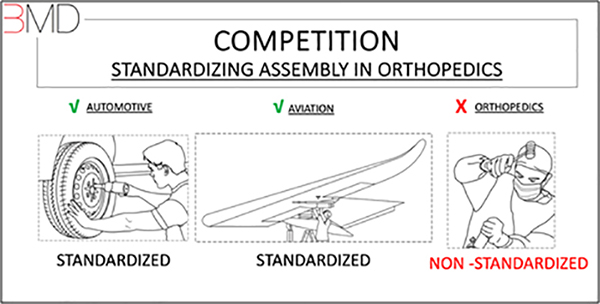
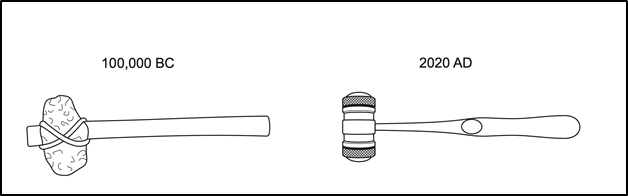
Orthopedic surgeons are a bit different from most other surgeons. Most surgeons typically dissect, cut, cauterize, and suture. Orthopedic surgeons do all of that, and in addition they apply large amounts of force to press fit implants to bone. During residency medical residents typically make fun of orthopedic residents by calling them “carpenters”, however, orthopedic surgeons are more appropriately likened to mechanics because most of the time they are assembling things with tools that deliver large amounts of force to the patient’s body. In that sense, orthopedic surgeons are like auto and aviation mechanics.
In these industries, there are strict standardization rules that are referred to as ISO, which applies to all aspects of the product including Materials, Design and Assembly.
Standardization ensures that every part, component, and assembly process adhere to strict guidelines and specifications. This helps maintain a high level of safety and reliability in the final product, reducing the likelihood of failure, defects and malfunction caused by inconsistencies and unproven practices.
This fact is never more relevant than today, as we see problems in aviation industry with assembly of airplane doors in the fuselage. We can all agree that we care equally as much about the material, design, and assembly of the plane in which we travel.
Assembly in Aviation
If we look at total hip replacement through this standardization lens, we can see that over the years (bio)materials and designs of implants have improved dramatically, however, the assembly process in orthopedics remains an enigma. Assembly in orthopedics remains a highly non-standardized and primitive process. There has been no improvement in this aspect of orthopedics.
In fact, four out of the five noted major problems in total hip replacement, namely aseptic loosening/periprosthetic fractures, mal-alignment, leg length discrepancy and metallosis can each be partly or wholly attributed to orthopedic surgeon’s non-standardized assembly technique.
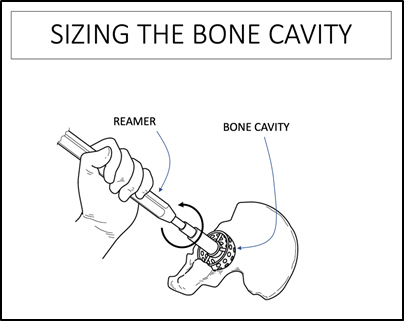
In orthopedic surgery we basically press fit (interference fit) implants into bone and modular implants into each other. Press fit technology dates back centuries of Persian and Greek early civilizations, who used various forms of interference fit in their construction. For example, in woodworking, joinery techniques involved fitting parts together tightly without use of fasteners, screws or nails. However, in these arenas, carpenters work with material that generally have homogenous material properties, and if they make a mistake and break the wood, they simply replace it.
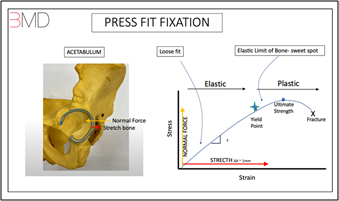
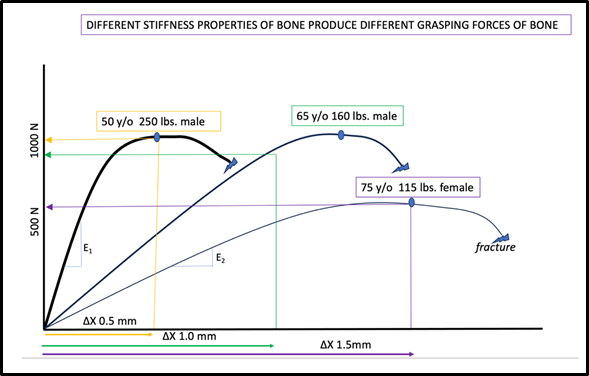
Conversely, in modern total hip replacement, we press fit metal implants, which are 10 to 20 times stiffer than bone, into a patient’s bone/body, that has vastly different strength and stiffness (modulus of elasticity) properties based on age and physiological condition.
We treat every patient the same regardless of age and bone quality. For example, regardless of age, we under- ream the acetabulum by 1mm and impact an acetabular cup that is one size larger.
But a 1mm under ream may be too little for a softer bone (you may need 2mm under ream to get a good press fit) and a 1mm under ream may be too much for a harder bone (you may only need 0.5mm under ream to get a good press fit).
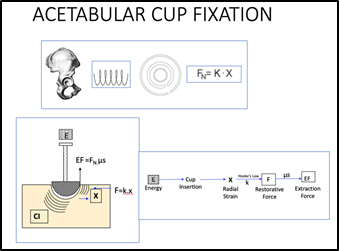
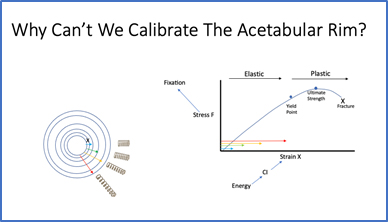
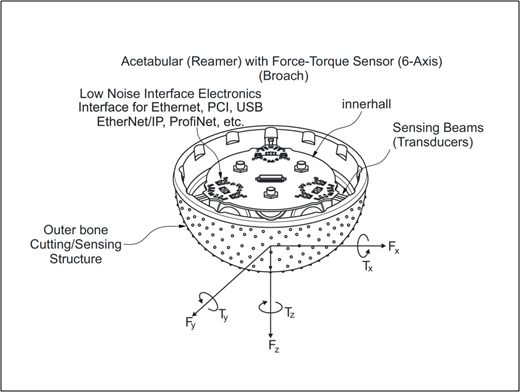
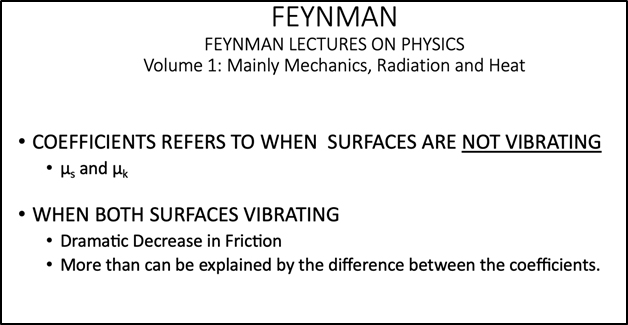
Basically, the grasping force of a bony cavity is FGrasp = FN. µs.
Where FN is the normal force at the implant/bone interface.
Wherein µs is the coefficient of static friction.
Based on Hooke’s law, FN is the product of modulus of elasticity of bone (K) and the radial strain or stretch of bone (∆X) at the implant bone interface. FN = (K. ∆X).
To get FGrasp correct, you must get FN correct. To get FN correct you must have an accurate sense of the values of K and X.
![]()

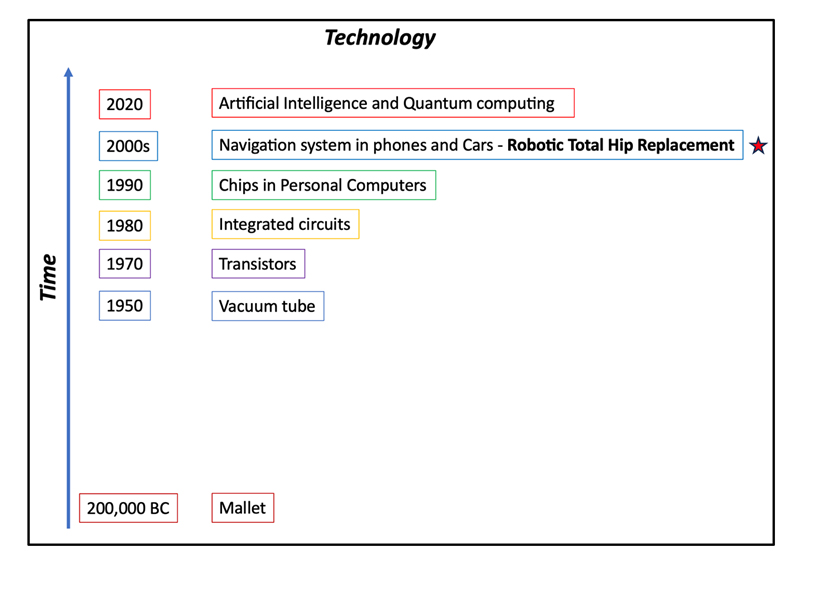
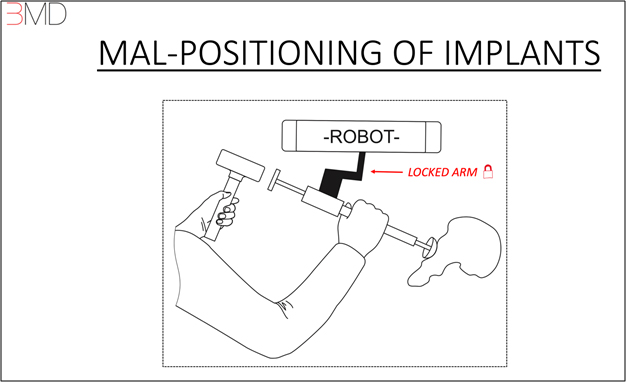
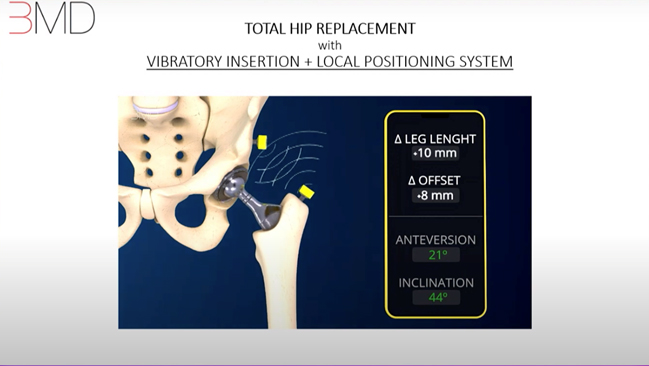
 In the late 1990s, the medical device community provided us with navigation and robotics to assist surgeons with visibility of the implant’s position (leg length, offset and alignment). However, as we discussed earlier, robotic platforms seem to have come at a great price. These platforms involve establishing a global positioning system in the OR space, which in turn involves too much bulk, extra workflow, too many glitches, too much human mechanical involvement including (screws, clamps, landmarking, registration, calibration), and line of sight issues. All of which add to compounding of errors, cost, time efficiency and most importantly cognitive load.
In the late 1990s, the medical device community provided us with navigation and robotics to assist surgeons with visibility of the implant’s position (leg length, offset and alignment). However, as we discussed earlier, robotic platforms seem to have come at a great price. These platforms involve establishing a global positioning system in the OR space, which in turn involves too much bulk, extra workflow, too many glitches, too much human mechanical involvement including (screws, clamps, landmarking, registration, calibration), and line of sight issues. All of which add to compounding of errors, cost, time efficiency and most importantly cognitive load.
 The best way to understand extended cognition is to study the behavior of spiders. When spiders build their webs, they wait to feel the vibrations in the web’s threads that are caused by struggling prey. When they sense movement of the threads, they move towards the direction of the signal. Spiders have a way of remembering the locations where the best foods were caught. In designing the future webs, spiders rather than remembering the locations that have done well, that is rather than storing these locations in their minds, the spiders weave this information into their web. In particular, they use their legs to tug on specific silk threads from which the prey has recently been detected, making them tighter. The tighter threads are more sensitive to vibrations, making future pray easier to detect on them. These alterations in the web offload some of the burden of cognition to its environment. Spiders expel their current knowledge and memory into a compact yet meaningful physical form. This interacting system of the spider and its web is smarter than the spider can hope to be on its own. This outsourcing of intellect to the environment is extended cognition. (Models of the Mind, Grace Lindsey).
The best way to understand extended cognition is to study the behavior of spiders. When spiders build their webs, they wait to feel the vibrations in the web’s threads that are caused by struggling prey. When they sense movement of the threads, they move towards the direction of the signal. Spiders have a way of remembering the locations where the best foods were caught. In designing the future webs, spiders rather than remembering the locations that have done well, that is rather than storing these locations in their minds, the spiders weave this information into their web. In particular, they use their legs to tug on specific silk threads from which the prey has recently been detected, making them tighter. The tighter threads are more sensitive to vibrations, making future pray easier to detect on them. These alterations in the web offload some of the burden of cognition to its environment. Spiders expel their current knowledge and memory into a compact yet meaningful physical form. This interacting system of the spider and its web is smarter than the spider can hope to be on its own. This outsourcing of intellect to the environment is extended cognition. (Models of the Mind, Grace Lindsey).